Shockwave Therapy Machine: What It Is, Uses & Benefits
- What is a shockwave therapy machine?
- Definition and core function of a shockwave therapy machine
- How shockwave therapy machines work
- Biological mechanisms behind the therapy
- Energy metrics: energy flux density and pulse characteristics
- Types of shockwave therapy machines
- Focused vs. radial shockwave therapy machines
- Typical technical differences between focused and radial machines
- Clinical uses of shockwave therapy machines
- Musculoskeletal conditions with good evidence
- Other emerging and specialty uses
- Evidence and outcomes: what the data shows
- Effectiveness by indication
- Typical treatment protocols and expected timeline
- Benefits of using a shockwave therapy machine in practice
- Non-invasive option with fast clinic throughput
- Cost-effectiveness and patient satisfaction
- Safety, contraindications and side effects
- Typical side effects and safety profile
- Contraindications to consider
- How to choose the right shockwave therapy machine for your clinic
- Clinical needs and device features to prioritize
- Economic and logistical considerations
- Practical tips for successful clinical implementation
- Patient selection and informed consent
- Training and protocol standardization
- Regulatory and reimbursement landscape
- Regulatory clearance varies by region and indication
- Reimbursement considerations
- FAQ — Common questions about shockwave therapy machines
- How many sessions are typically needed with a shockwave therapy machine?
- Does the treatment hurt when using a shockwave therapy machine?
- Are results from a shockwave therapy machine permanent?
- Is one type of shockwave therapy machine better than another?
- What safety checks should clinics perform before buying a shockwave therapy machine?
- Where can I learn more about clinical protocols for a specific device?
- Closing thoughts
- Why integrating a shockwave therapy machine can be valuable for modern clinics
- Additional FAQ — quick reference
- Can shockwave therapy machines replace surgery?
- Is shockwave therapy suitable for athletes?
- How should clinics measure success after treatment?
What is a shockwave therapy machine?
Definition and core function of a shockwave therapy machine
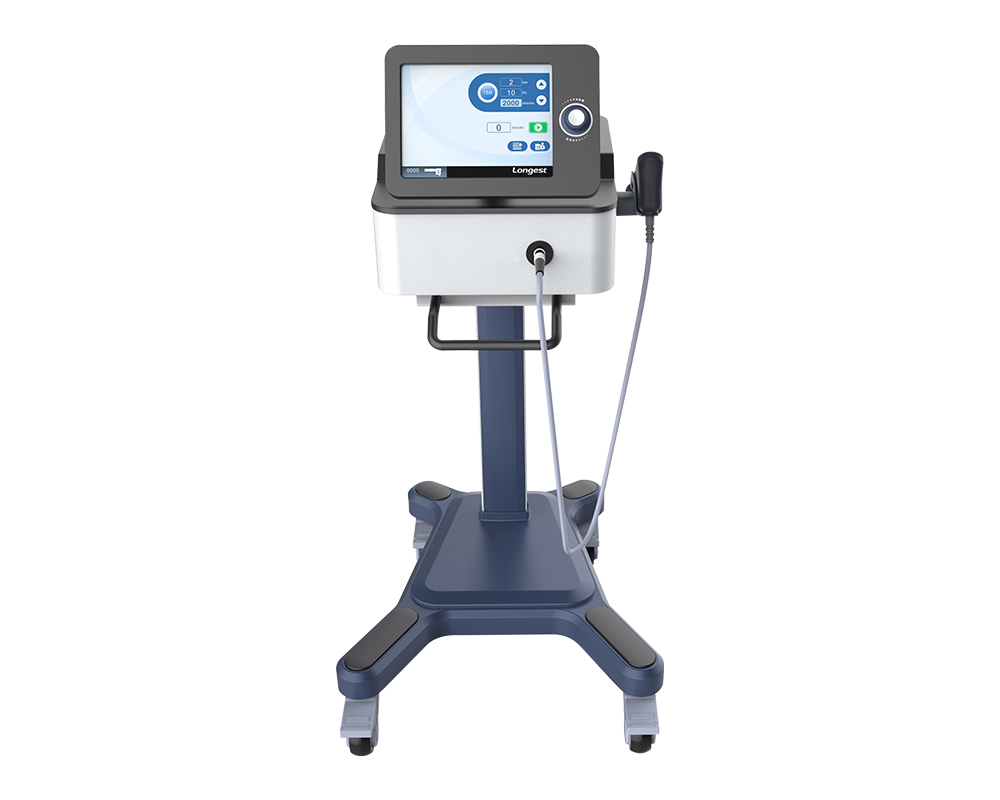
A shockwave therapy machine delivers short, high-pressure acoustic pulses (shockwaves) to targeted tissue to stimulate repair and reduce pain. Often referred to as extracorporeal shock wave therapy (ESWT), these systems are used in clinics, sports medicine centers, orthopedics, physiotherapy and urology clinics. The term shockwave therapy machine is commonly used across product literature and clinical protocols.
How shockwave therapy machines work
Biological mechanisms behind the therapy
Shockwave therapy machines work by creating mechanical stress in tissue that triggers biological responses: increased local blood flow, stimulation of angiogenesis, modulation of inflammation, and activation of cellular repair pathways. At therapeutic energy levels, shockwaves can break up calcifications and encourage tissue remodeling without open surgery.
Energy metrics: energy flux density and pulse characteristics
Key technical metrics include energy flux density (EFD, measured in mJ/mm²), number of pulses per session, frequency (Hz), and waveform. Clinical practice commonly categorizes EFD as low (<0.08 mJ/mm²), medium (0.08–0.28 mJ/mm²) and high (>0.28 mJ/mm²). These values guide protocols for different indications and tissue depths.
Types of shockwave therapy machines
Focused vs. radial shockwave therapy machines
There are two primary types of shockwave therapy machines: focused and radial. Focused devices concentrate energy at a depth and can reach deeper structures; radial systems deliver broader, surface-level mechanical pressure. Both have clinical roles depending on the target tissue.
Typical technical differences between focused and radial machines
Below is a concise comparison table to help clinicians and buyers understand practical differences between device types.
| Feature | Focused shockwave machine | Radial shockwave machine |
|---|---|---|
| Energy delivery | High peak pressure concentrated at focal point | Lower peak pressure, broader surface impact |
| Typical penetration depth | Typically up to ~8–10 cm (depends on applicator) | Typically up to ~3–4 cm |
| Usual EFD ranges | Often medium to high EFD (0.08–0.60+ mJ/mm²) | Usually low to medium EFD (<0.28 mJ/mm²) |
| Best clinical uses | Deep tendinopathies, calcific deposits, bone indications | Superficial tendinopathies, muscle trigger points, broader soft-tissue use |
| Typical session pulses | 1,000–3,000 pulses | 1,000–3,000 pulses |
Clinical uses of shockwave therapy machines
Musculoskeletal conditions with good evidence
Shockwave therapy machines are widely used and supported by clinical studies for several musculoskeletal indications. Key examples include:
- Plantar fasciitis — multiple randomized trials and meta-analyses report meaningful pain reduction and functional improvement. Typical success rates range from ~60% to 80% in chronic cases.
- Lateral epicondylitis (tennis elbow) — ESWT can reduce pain and improve grip strength in chronic patients resistant to conservative care.
- Achilles and patellar tendinopathy — many studies show pain and functional gains, particularly using focused shockwaves for deeper tendon lesions.
- Calcific rotator cuff tendinopathy — shockwaves help fragment calcium deposits and speed symptom resolution; reported improvement rates often exceed 70% in treated cohorts.
- Delayed and non-union fractures — high-energy focused shockwaves have been used to stimulate bone healing in selected cases.
Other emerging and specialty uses
Low-intensity shockwave therapy (LiSWT) is being investigated for erectile dysfunction (ED), chronic wounds, and certain dermatology indications. Clinical trials for ED show improvements in erectile function scores in some patient groups, but regulatory approvals and consensus vary by region and device.
Evidence and outcomes: what the data shows
Effectiveness by indication
Systematic reviews indicate that shockwave therapy machines provide clinically significant benefits for chronic plantar fasciitis and certain tendinopathies compared with sham or conservative treatment. Results are heterogeneous—outcomes depend on device type, EFD, number of sessions, and patient selection. For many conditions, reported improvement rates commonly cluster between 50% and 80% in appropriately selected patients.
Typical treatment protocols and expected timeline
Common protocols involve 1,500–3,000 pulses per session, delivered at 1–4 weekly intervals for 1–6 sessions. Pain relief often begins within weeks but maximal functional gains may require months as tissue remodeling continues. For bone-related indications, higher-energy protocols with fewer sessions are typically used under specialist supervision.
Benefits of using a shockwave therapy machine in practice
Non-invasive option with fast clinic throughput
One major clinical benefit of a shockwave therapy machine is offering a non-invasive alternative to injections or surgery for many chronic conditions. Sessions are brief (10–20 minutes), allowing efficient clinic workflows.
Cost-effectiveness and patient satisfaction
While device investment is significant, shockwave therapy can reduce long-term costs by avoiding surgeries and repeated injections. Patient satisfaction is often high when pain and function improve, and many clinics report good reimbursement pathways depending on regional payer policies.
Safety, contraindications and side effects
Typical side effects and safety profile
Shockwave therapy machines are generally safe. Common transient side effects include mild pain during treatment, local bruising, transient swelling, and erythema. Serious adverse events are rare when devices are used according to protocols.
Contraindications to consider
Contraindications commonly include: pregnancy, active infection at the treatment site, coagulation disorders or ongoing anticoagulation without clearance, malignant lesions in the treatment area, and open growth plates in children. Always review device-specific safety instructions and local regulations.
How to choose the right shockwave therapy machine for your clinic
Clinical needs and device features to prioritize
Select a shockwave therapy machine that matches your most common indications. Key procurement factors include: whether you need focused or radial waves (or both), adjustable EFD, a range of applicators, treatment protocols that can be saved, portability, service/warranty terms, and local regulatory clearance for intended indications.
Economic and logistical considerations
Device costs vary widely — from tens of thousands for basic radial systems to higher prices for multi-modal focused devices with advanced generators and imaging integration. Factor in consumables, service contracts, staff training, and expected patient throughput to calculate return on investment.
Practical tips for successful clinical implementation
Patient selection and informed consent
Choose patients with chronic, well-defined pathology who have not responded to conservative care. Review realistic expectations, discuss the number of sessions, possible discomfort, and alternative treatments. Document consent and baseline outcome scores (e.g., pain scales, functional questionnaires).
Training and protocol standardization
Ensure clinicians receive manufacturer training and follow evidence-based protocols. Standardize session parameters (EFD, pulses, frequency) for each indication and monitor outcomes to refine local protocols.
Regulatory and reimbursement landscape
Regulatory clearance varies by region and indication
Regulatory status of shockwave therapy machines depends on the device model, intended use, and jurisdiction. In many countries, devices are cleared for specific musculoskeletal indications; for other uses (e.g., ED), regulatory acceptance is variable. Verify local approvals before marketing or using a device clinically.
Reimbursement considerations
Insurance coverage for shockwave therapy differs across payers and regions. Some musculoskeletal indications receive reimbursement; others may be out-of-pocket. Clinics should document outcomes and codes to support reimbursement requests.
FAQ — Common questions about shockwave therapy machines
How many sessions are typically needed with a shockwave therapy machine?
Most protocols call for 1–6 sessions, typically spaced weekly. For many chronic tendinopathies, 3 sessions spaced 1 week apart is common; more sessions may be used depending on response.
Does the treatment hurt when using a shockwave therapy machine?
Patients can experience discomfort during application; clinicians often adjust energy, use local anesthetic selectively (though anesthetic may blunt biological effects), or tailor protocols to tolerance.
Are results from a shockwave therapy machine permanent?
Many patients achieve long-term symptom relief, but outcomes depend on the underlying condition, patient factors, and adherence to rehabilitation. Shockwave therapy often accelerates healing and reduces pain, but no treatment guarantees permanent cure in every case.
Is one type of shockwave therapy machine better than another?
No single device is universally best. Focused machines are preferable for deeper or calcific lesions; radial machines are efficient for superficial soft-tissue problems. Multi-mode systems or clinics with clear indication focus can optimize treatment choices.
What safety checks should clinics perform before buying a shockwave therapy machine?
Confirm regulatory clearance for your intended uses, request clinical evidence and peer-reviewed data from the manufacturer, review warranty and service contracts, and plan staff training. Also validate consumable costs and expected clinic throughput to justify purchase.
Where can I learn more about clinical protocols for a specific device?
Refer to the manufacturer's clinical white papers, peer-reviewed studies using that device model, and professional society guidance. Manufacturer training and local clinical collaborations are valuable for protocol development.
Closing thoughts
Why integrating a shockwave therapy machine can be valuable for modern clinics
When used appropriately, a shockwave therapy machine offers a non-invasive, evidence-supported option for many chronic musculoskeletal conditions and emerging indications. Success depends on correct device selection, standardized protocols, patient selection, and proper clinician training. For clinics considering purchase, balance clinical goals, device capabilities, regulatory status, and economic planning to maximize patient outcomes and return on investment.
Additional FAQ — quick reference
Can shockwave therapy machines replace surgery?
For many chronic soft-tissue problems, shockwave therapy may reduce the need for surgery, but it does not replace surgery in all cases—surgical referral may still be necessary for advanced structural pathology.
Is shockwave therapy suitable for athletes?
Yes. Athletes often benefit from accelerated recovery and conservative management offered by shockwave therapy machines; protocols should be integrated with rehabilitation.
How should clinics measure success after treatment?
Use validated patient-reported outcome measures (e.g., pain VAS, functional scales), objective strength/range assessments, and patient satisfaction surveys. Track outcomes over months to capture sustained benefit.
Active Passive Trainer Cost in UK: Prices, Buying Guide & Where to Buy
Wholesale electrical muscle stimulation device manufacturer and supplier
Buying Guide: Choosing the Right Shockwave Therapy Machine
Top 10 medical device Manufacturers and Supplier Brands
LGT-2201DVT
When are DVT pumps used?
DVT pumps are commonly used in hospitals after surgery or for individuals at risk of developing blood clots. They can be used prophylactically to prevent DVT or therapeutically to treat existing clots.
2510A physical therapy
Can shockwave treatment be combined with other therapies?
Shockwave treatment can be combined with a variety of therapies. For example, when combined with physical therapies such as electrotherapy and laser, it can improve circulation, repair tissues, and relieve pain. It can also be combined with rehabilitation therapies such as rehabilitation training and deep muscle massage to accelerate the patient's rehabilitation process and improve the quality of life. However, the specific treatment plan should be formulated according to the specific condition and individual differences of the patient.
2510A-beauty
In which circumstances is AWT not suitable?
Pregnancy
Over major blood vessels and nerves
Having pacemakers or other implanted devices
Open wounds Taking oral anti - coagulants
Having a blood clotting disorder
Having received a Steroid injection within 6 weeks
Tumors are present at the treatment site
Having skin infection or abrasion at the treatment site
Electrostatic Oscillation
Who is not suitable to use this device?
It is not recommended for people with metal implants (such as pacemakers), pregnant women, open wounds or severe skin diseases. Before use, if you have any health concerns, it is recommended to consult a professional doctor first.
LGT-2660AP/BP Magnetic Stimulator
Can the LGT-2660AP/BP Electromagnetic Stimulator be used in home settings?
No, the LGT-2660AP/BP is a professional clinical device. It requires operation by trained medical or rehabilitation professionals, so it is intended for use in hospitals, clinics, rehab centers, and sports medicine facilities.

Electrical Extracorporeal Shock Wave Therapy Device PowerShocker LGT-2500S
The LGT-2500S is a portable, tabletop extracorporeal shock wave therapy (ESWT) device. It effectively stimulates the healing of troublesome tissue, alleviates pain, and non-invasively supports the recovery of the patient's tissue. It is a completely natural and drug-free option for various conditions in physiotherapy, veterinary medicine, and aesthetic medicine.

Electromagnetic Stimulator for Musculoskeletal Rehabilitation LGT-2660AP/BP
The LGT-2660 Series Electromagnetic Stimulator for Musculoskeletal Pain is an advanced rehabilitation device engineered to address a wide range of musculoskeletal pain conditions and associated dysfunctions. Operating on the principle of electromagnetic induction, it generates induced currents to regulate neuromuscular function while delivering deeply penetrating energy—this energy transcends superficial tissues to act directly on muscles, joints, and bones. For both acute and chronic musculoskeletal pain, it provides a safe, efficient, and medication-free new solution.

Professional 12-Channel Low-Frequency Electrical Stimulation Machine LGT-2320SP
LGT-2320SP is an advanced electrical stimulation sports training station. It leads to multisite high-efficiency strength gain and realizes bilateral balanced development with motor point detection.
Specifically designed for sports medicine professionals, this device is ideal for the treatment and rehabilitation of sports-related injuries. It delivers precise electrical impulses to targeted areas of the body, promoting pain relief, muscle strengthening, and accelerated recovery.

Electromagnetic Stimulator for Pelvic floor rehabilitation LGT-2640AP
The LGT-2640AP Pelvic Floor Magnetic Stimulator is a precision rehabilitation device designed for targeted pelvic floor therapy. Featuring 24 visualized preset protocols (paired with anatomical diagrams), customizable treatment plans, and a pre-adaptation function, it delivers non-invasive, painless stimulation to support postpartum recovery, male pelvic floor rehabilitation, and geriatric pelvic health.
© 2025 Longest Medical. All Rights Reserved. Powered by gooeyun.






LongestMedical
LongestGloba
longest
guangzhou_longest
GzLongest